The integrative medicine approach that combines conventional and alternative therapies with an emphasis on natural, less invasive, evidence-based option is well suited for the management of diabetes.
Diabetes is a chronic condition that affects the way the body processes blood sugar (glucose). Integrative medicine can play a significant role in managing diabetes by combining conventional medical treatments with complementary therapies and lifestyle modifications. Here are some ways integrative medicine can help manage diabetes:
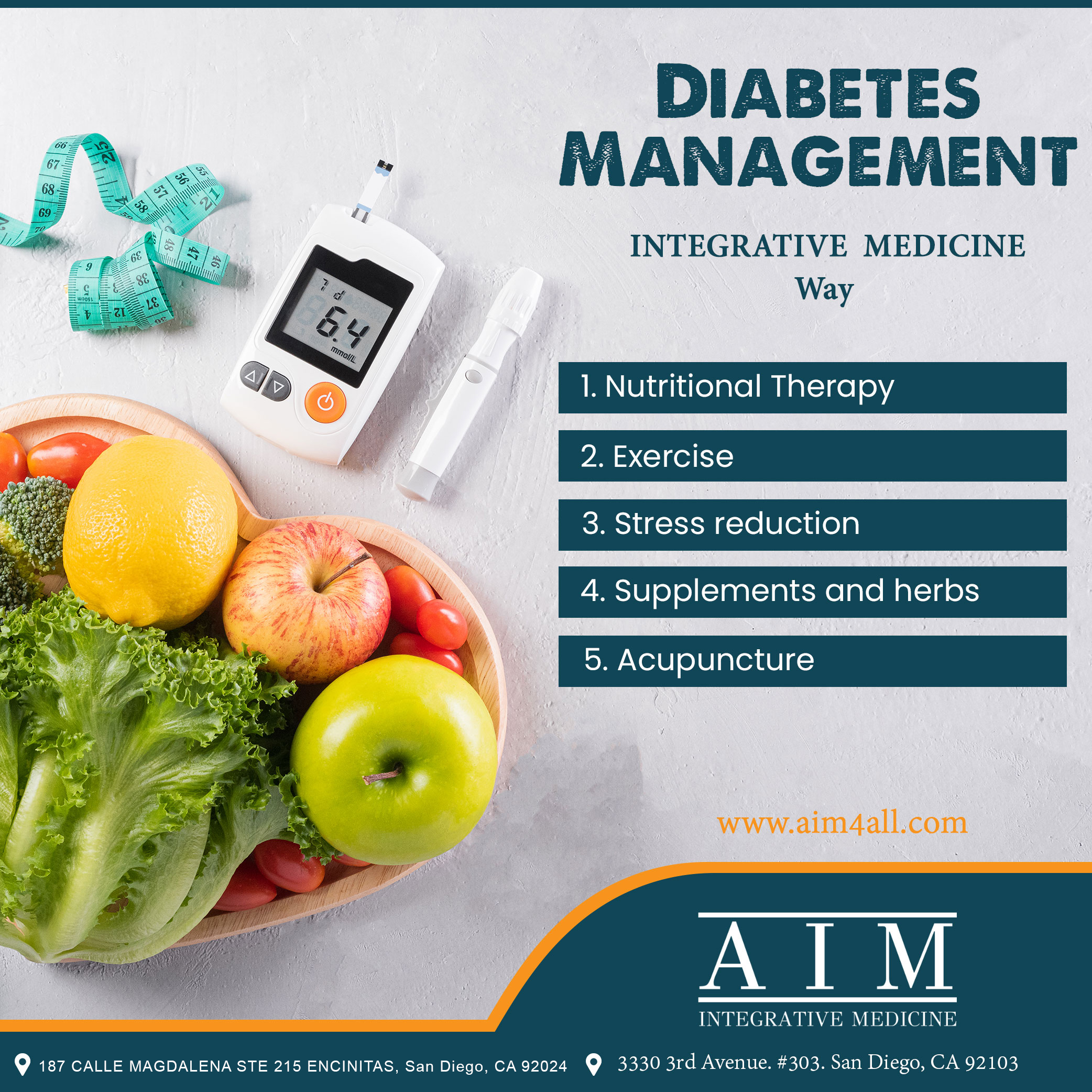
- Nutritional therapy: A healthy diet is critical for managing diabetes. Integrative medicine practitioners can recommend a personalized diet plan that focuses on nutrient-dense foods, avoiding processed foods, and controlling portion sizes.
- Exercise: Regular physical activity is essential for maintaining blood sugar levels, managing weight, and reducing the risk of complications. Integrative medicine practitioners can recommend an exercise plan that is tailored to an individual’s needs and fitness level.
- Stress reduction: High levels of stress can cause blood sugar levels to spike, making it more challenging to manage diabetes. Integrative medicine can incorporate stress reduction techniques such as mindfulness meditation, yoga, and tai chi.
- Supplements and herbs: Certain supplements and herbs can be helpful in managing diabetes. For example, chromium supplements can improve insulin sensitivity, while cinnamon can help lower blood sugar levels.
- Acupuncture: Acupuncture is a complementary therapy that can help manage diabetes by reducing stress, improving insulin sensitivity, and promoting relaxation.
It is important to note that integrative medicine should not replace conventional medical treatment for diabetes. However, incorporating integrative approaches into a comprehensive diabetes management plan can help improve outcomes and overall health. It is essential to work with a qualified integrative medicine practitioner and a healthcare team to ensure safe and effective treatment.
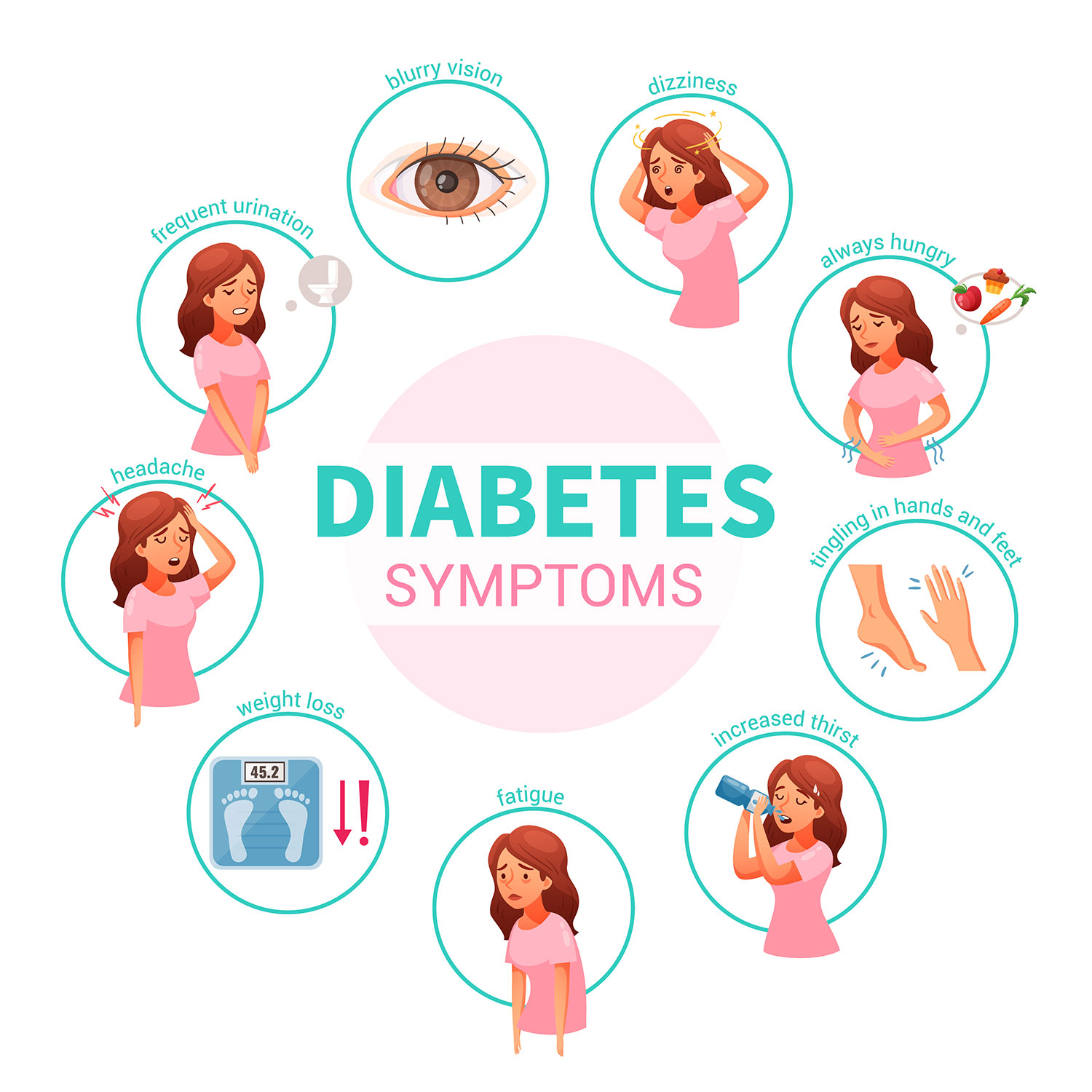
Diabetes Symptoms | AIM4ALL Integrative Medicine
An integrative medicine approach to diabetes
Traditional diabetes care management often focuses solely on the management of blood sugar levels and the prevention of complications. This typically involves regular monitoring of blood sugar levels, adjustment of medication doses, and management of any complications that arise.
In contrast, the integrated medicine approach to diabetes management takes a holistic view of the patient’s overall health and well-being. This approach recognizes the interconnectedness of physical, mental, and emotional health and seeks to address all of these aspects in order to improve the patient’s quality of life.
The integrated medicine approach also incorporates a wider range of treatments, including both conventional and alternative therapies. This allows for a more personalized approach to treatment, as the doctor can tailor the treatment plan to the individual’s unique needs and circumstances.
Understanding Diabetes
There are two types of diabetes: type 1 and type 2.
- Type 1 Diabetes: In type 1 diabetes, the body’s immune system attacks and destroys the cells in the pancreas that produce insulin. This means that the body is unable to produce enough insulin to regulate blood sugar levels, and as a result, people with type 1 diabetes must take insulin injections to control their blood sugar. The peak age for being diagnosed with type 1 is 14 years old.
- Type 2 Diabetes: In type 2 diabetes, the body’s cells become resistant to the effects of insulin, which means that the body must produce more insulin in order to keep blood sugar levels under control. The peak age of diagnosis is 45.
In general, type 1 diabetes is considered to be an autoimmune disorder, while type 2 diabetes is a metabolic disorder. The integrative medicine approach to diabetes focuses on treating and reversing type 2 diabetes, but it also addresses the underlying problem of insulin resistance generally.
This problem is more widespread than you would think, and insulin resistance can show up in blood tests decades before an actual diagnosis of diabetes is made. A study published last year in the Journal of Clinical Endocrinology and Metabolism found that nearly 40 percent of young adults have insulin resistance, raising the risk of cardiovascular disease later in life.
What is the integrative medicine approach to diabetes?
What is Integrative Medicine Protocol For Reversing Type 2 Diabetes?
While these statistics sound frightening, there is good news. While genetics does play a role in type 2 diabetes, this condition is primarily driven by lifestyle and environmental factors you can control.
Type 2 diabetes, sometimes called non-insulin-dependent diabetes, is a chronic metabolic condition marked by elevated blood glucose (sugar) levels brought on by the body’s ineffective use or insufficient production of the hormone insulin. Insulin, produced by the pancreas, controls blood sugar levels by allowing glucose to enter the cells to be used as energy.
Type 2 diabetes is when your cells don’t respond normally to insulin, resulting in insulin resistance. The pancreas cannot produce enough insulin to keep blood sugar levels in normal ranges. It’s called non-insulin-dependent diabetes because the body can still make and use insulin, albeit ineffectively. Lifestyle factors are the primary driver of this condition.
What Causes Type II Diabetes?
- Being overweight or obese increases your risk of developing insulin resistance, which can lead to type 2 diabetes.
- Lack of exercise and a sedentary lifestyle can contribute to insulin resistance and lead to type 2 diabetes.
- A diet high in refined and processed foods, sugar, and unhealthy fats increases your risk of developing type 2 diabetes. Various nutrient deficiencies or insufficiencies are associated with type 2 diabetes, including inositol (a sugar produced by the body that supports blood glucose and insulin regulation), Vitamin D, and micronutrients (including zinc, chromium, and magnesium).
- If you have a family history of diabetes, you’re at higher risk of developing the condition yourself.
- The risk of developing type 2 diabetes increases in people over 45.
- People of certain ethnicities, including Black, Hispanic, Native American, Asian American, or Pacific Islander, have a higher risk of developing type 2 diabetes.
- Women who have had gestational diabetes (diabetes during pregnancy) are at higher risk of developing type 2 diabetes later in life.
- Those with blood sugar levels above normal but not high enough to be in diabetic ranges (prediabetes) are at higher risk of developing type 2 diabetes.
- Disruption of the gut microbiome (the trillions of microorganisms that live in the gastrointestinal tract), called dysbiosis, is associated with this condition.
- Evidence indicates that the toxins increase the risk for type 2 diabetes. This includes toxins such as Bisphenol A (BPA, a chemical used to produce plastics), arsenic, dioxin, and others, many commonly found in pesticides.
- The circadian rhythm is the body’s internal 24-hour clock that syncs up with our daily light and dark cycles. Disruption in the circadian rhythm is associated with type 2 diabetes, which includes disruption to regular sleep patterns.
It’s important to note that having one or more of these risk factors doesn’t necessarily mean you’ll develop type 2 diabetes, but it’s essential to be aware of them and make lifestyle changes to reduce your risk.
Recent Comments